Overactive Bladder
Symptoms & Causes
Treatments & Procedures
Overview
An Overactive Bladder is a combination of symptoms that cause a sudden urge to urinate and possible incontinence. The risk of an overactive bladder increases with age, primarily affecting women and men over the age of 40. Other risk factors include menopause and diseases that affect the nervous system, such as stroke and multiple sclerosis.
Symptoms
Common symptoms associated with an overactive bladder include:
• Urinary frequency - urinating more often that you would like • Urinary urgency – sudden need to urinate • Urinary incontinence - loss of urinary control • Visiting the restroom to urinate more than eight times a day
Should you experience any of these symptoms, an exam, and consultation are the next practical step.
Causes
There are many different health issues that can contribute to overactive bladder, including the following:
• Excess caffeine or alcohol intake • Excess urine production (including fluid intake or medical conditions) • Neurologic disorders or damage (including stroke and multiple sclerosis) • Diabetes • Hormonal changes around menopause in women • Weak or spastic pelvic muscles • Urinary tract infection (UTI) • Drug side effects • Bladder abnormalities (such as tumors or bladder stones) • Enlarged prostate in men • Constipation • Declining cognitive function associated with age
Millions of Americans, up to 30% of men and up to 60% of women, are affected by an overactive bladder (OAB). Worldwide, this condition is highly prevalent and negatively impacts the sufferer’s quality of life. Because many living with OAB don’t ask for help out of embarrassment, the actual number of cases is likely higher.
Overactive Bladder Care at Integrative Urology
Treatment
The first step to treating an overactive bladder is correct diagnosis. Diagnosis of overactive bladder requires a physical exam of the lower abdomen, the rectum, and the prostate in men. To evaluate your medical history, we may ask you questions concerning the severity and duration of your symptoms, which medications you are taking, your dietary habits, and past or current health issues. We may also ask you to keep a bladder diary. This aid to diagnosis requires patients to keep track of how much fluid they consume, how many times they go to the restroom, any incidents of urinary incontinence, and when these incidents occur (for example, when laughing or coughing).
Other tests to diagnose overactive bladder include: • Urine cultures • External bladder scans • Cystoscopy • Urodynamic testing • A symptom questionnaire
Treatment for overactive bladder can be as simple as making a few lifestyle changes. Attention to diet is important because certain foods and drinks can make symptoms worse. Spicy foods, citrus fruits and juices, tomatoes and tomato products, coffee, tea, and alcoholic beverages should be avoided. Patients should also consider quitting smoking and exercising regularly. Strengthening the pelvic floor muscles with Kegel exercises may also help reduce or prevent instances of incontinence. If you experience urinary incontinence, you may wish to use various products and devices, such as special underwear, pads, and internal bladder support for women, to manage leakage and inconvenient incidents. Other treatment options include medical and surgical procedures including InterStim™ and BOTOX® for the bladder.
Percutaneous Tibial Nerve Stimulation (PTNS)
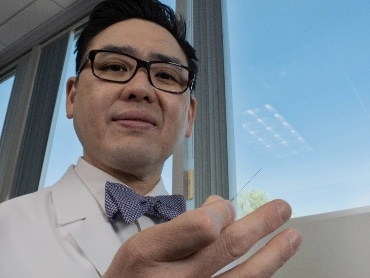
Percutaneous Tibial Nerve Stimulation (PTNS) is a popular treatment for urinary frequency and overactive bladder. It involves neuromodulation (modifying nerve signals) of the tibial nerve, which runs up the leg and communicates with nerves involved in bladder function. From a sitting position, one or more thin needles are placed in the lower leg to stimulate the tibial nerve, similar to acupuncture. Electrostimulation is performed weekly for a brief period in a painless fashion for a 12-week treatment course. During the PTNS therapy treatment course, patients experience significant improvement in urinary frequency, urgency and incontinence, which are usually durable after the treatment course. PTNS is considered safe and effective for patients who have failed conservative measures such as dietary changes and medications or cannot tolerate medication and wish to avoid surgery. Having trained in acupuncture in China and the United States, Dr. Mark Hong incorporates knowledge of traditional Chinese Medicine in his personalized PTNS treatments to achieve the best possible results.

Benefits:
Minimally Invasive
No Ongoing Medication
Surgery Free
Quick Treatment
InterStim™
InterStim™ Therapy is an FDA-approved treatment for overactive bladder and urinary retention. A small implantable neurotransmitter device is implanted that sends electrical impulses to nerves (sacral nerves) in the lower back. These nerves are then stimulated gently to decrease the symptoms of OAB. This proven treatment is for people who have not had success with traditional bladder control treatments such as medication and physical therapy.
There is a short trial period of 3-7 days to see if InterStim™ is right for you. Patients are fitted with an external device. During your trial period, you will keep track of your urinary symptoms in a bladder diary. If your symptoms are significantly reduced or eliminated during the testing period, you may benefit from implantation of the InterStim™ device.
InterStim™ placement is a quick outpatient procedure and usually takes between 20-30 mins to complete.
Benefits:
Minimally Invasive
Quick 20-30 minutes
BOTOX®
Botox® works by temporarily paralyzing the muscles that cause OAB and urinary incontinence, allowing the bladder to hold more urine and reducing the frequency and urgency of urination. The procedure involves injecting Botox® directly into the bladder muscle using a cystoscope, a thin tube with a camera and light at the end. The treatment is relatively quick and can be performed in the office under local anesthesia. Botox® is a good treatment for an overactive bladder because it can provide relief without the need for invasive surgery or medication. There are several factors to determine if Botox® is right for you, such as medical history, current medications, and your overall health status.
